INTERNSHIP ASSESSMENT: Posted in GENERAL MEDICINE department from 12/12/22 to 11/2/23 . In OP: Took brief history of the patients , done systemic examination (CVS, CNS, RESPIRATORY, PER ABDOMEN). Ordered necessary investigations according to the symptoms. Learnt to prescribe medications according to the symptoms of the patient. UNIT DUTY: Drawn venous blood samples , collected reports of the samples sent. Got blood culture bottles and swabs from the lab and collected culture reports from microbiology department. Updated the reports in WhatsApp groups, investigation charts Updated the fever charts everyday. Got the ECG , 2D echo , x rays done for the patients. Initiated and monitored blood transfusion of a patient. Monitored vitals of the patients in the ward , ICU , AMC. Typed and printed discharge summaries of the patients BLOGS OF THE PATIENTS ADMITTED UNDER THE UNIT . https://keshithakonda.blogspot.com/2023/01/this-is-online-e-log-book-to-discuss_11.html This is a case of 60 F ...
Popular posts from this blog
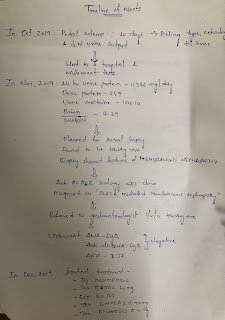
This is a online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patients problems through series of inputs from available global community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This E log book also reflects my patient centered online learning portfolio and your valuable inputs in comment box is welcome. I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history , clinical findings , investigations and come up with diagnosis and treatment plan . 45 year old male cane with the chief complaints of burning sensation of feet and tingling sensation in feet on and off since 2 months. Timeline of events : In OCT 2019: Patient was apparently asymptomatic 3 years back , then h...
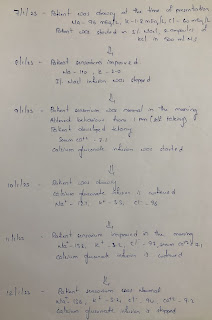
60 year female with altered sensorium secondary to dyselectrolytemia
This is a online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patients problems through series of inputs from available global community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This E log book also reflects my patient centered online learning portfolio and your valuable inputs in comment box is welcome. I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history , clinical findings , investigations and come up with diagnosis and treatment plan . CHIEF COMPLAINTS: Vomiting since 4 days Generalised weakness since 4 days Facial puffiness since 3 days Decreased urine output since 3 days HOPI : Patient was apparently asymptomatic 4 days ago, then she had vomitings 3-4 epis...












































Comments
Post a Comment