60 year female with altered sensorium secondary to dyselectrolytemia
This is a online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patients problems through series of inputs from available global community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs .This E log book also reflects my patient centered online learning portfolio and your valuable inputs in comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history , clinical findings , investigations and come up with diagnosis and treatment plan .
CHIEF COMPLAINTS:
Vomiting since 4 days
Generalised weakness since 4 days
Facial puffiness since 3 days
Decreased urine output since 3 days
HOPI :
Patient was apparently asymptomatic 4 days ago, then she had vomitings 3-4 episodes/day , food as content,non projectile , non bilious associated with abdominal pain .
Facial puffiness and decreased urine output since 3 days.
Cough since 4 years , on and off, productive ,scanty white coloured sputum with no diurnal variation, more during winter season.SOB of grade 2 since 4 years more in supine position and during winter .
Burning micturition and decreased stream of urine since 4 days.No C/O hesitancy , dribbling.
No H/O orthopnea, PND, chest pain.
PAST HISTORY:
Not a k/c/o DM , HTN , epilepsy, asthma , CAD , CVD,TB
Hysterectomy 20 years ago.
PERSONAL HISTORY:
Appetite-Decreased
Diet - Mixed
Bowel - Regular
Bladder - burning micturition and decreased stream of urine.
Sleep - Decreased.
General examination:
Patient is conscious, coherent, cooperative, well oriented to time , place and person
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy- absent
Pedal edema - pitting type extending till knee
VITALS : Temp - 98.6 F
PR - 94 bpm
BP - 120/70 mmhg
RR - 18 cpm
SPO2 - 98% onRA
GRBS - 102 mg/dl
Systemic examination:
CENTRAL NERVOUS SYSTEM:on the day of presentation
Conscious,coherent and cooperative
Speech- normal
No signs of meningeal irritation.
Cranial nerves- intact
Sensory system- normal
Motor system:
Tone- normal
Power- bilaterally 5/5
Reflexes Right Left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
CNS examination - on 11/1/23.
GCS - E2 V3 M4
Right. Left.
TONE
UL. HYPOTONIA HYPOTONIA
LL HYPOTONIA. HYPOTONIA
POWER
UL. 2/5. 2/5
LL. 2/5. 2/5
REFLEXES
BICEPS - NEGATIVE NEGATIVE
TRICEPS- NEGATIVE. NEGATIVE
SUPINATOR-NEGATIVE. NEGATIVE
KNEE - NEGATIVE. NEGATIVE
ANKLE NEGATIVE. NEGATIVE
BABINSKI MUTE. MUTE
CNS EXAMINATION ON 12/1/23:
GCS - E4 V5 M6
Right. Left.
TONE
UL NORMAL. NORMAL
LL . NORMAL NORMAL
POWER
UL. 5/5. 5/5
LL. 5/5 5/5
REFLEXES
BICEPS - 1+ 1+
TRICEPS- 1+. 1+
SUPINATOR-1+. 1+
KNEE - 1+. 1+
ANKLE . 1+. 1+
BABINSKI FLEXION. FLEXION
PER ABDOMEN:
Inspection :
Umbilicus is central and inverted
All quadrants are moving equally with respiration
No scars , sinuses , engorged veins, visible pulsations .
Hernial orifices are free.
Palpitation :
Abdomen is soft and non tender .
No organomegaly.
Percussion :
Tympanic note heard over the abdomen.
Auscultation:
Bowel sounds are heard.
CARDIOVASCULAR SYSTEM:
Inspection:
Shape of chest is elliptical.
No raised JVP
No visible pulsations, scars , sinuses , engorged veins.
Palpitation:
Apex beat - felt at left 5th intercostal space
No thrills and parasternal heaves
Auscultation :
S1 and S2 heard.
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical ,
Both sides moving equally with respiration .
No scars, sinuses, engorged veins, pulsations
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present. Normal vesicular breath sounds heard.
INVESTIGATIONS:
Hb – 8.4 gm/dl
TLC – 5900 cells/cu mm
Neutrophils : 77
Lymohocytes : 12
Eosinophils : 01
Monocytes : 10
Platelets – 2.14 lakhs/cu mm
CUE :
Albumin - traces
Pus cells - 2-3/HPF
Epithelial cells - 2-3/HPF
RENAL FUNCTION TESTS :
Urea : 24 mg/dl
Creatinine : 1.6 mg/dl
Sodium : 96 mEq/L
Potassium : 1.8 mEq/L
Chloride : 60 mEq/L
LIVER FUNCTION TESTS :
Total bilirubin : 1.54 mg/dl
Direct bilirubin : 0.38 mg/dl
AST : 116 IU/L
ALT : 46 IU/L
Alkaline phosphate :162 IU/L
Total proteins :5.6 gm/dl
Albumin : 3.6 gm/dl
A/G ratio : 1.81
Serum osmolality : 192.4
On 8/1/23:
On 10/1/23:
Morning:
Evening:
On 11/1/23:
On 12/1/23:
Serum calcium : 9.2
Serum phosphorus:3.5
Serum magnesium:1.7
24hr urine sample : volume - 3800 ml
Calcium - 228 mg/day
Sodium -646 mmol/day
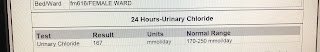
Chloride - 532 mmol/day
Phosphorus- 0.30gm/day
Spot urine protein :8
Spot urine creatinine :14.1
Ratio : 0.55
CXR : on the day of admission
On 10/1/23:
ECG :on the day of admission
USG :
TROUSSEAU’s SIGN :
PROVISIONAL DIAGNOSIS:
ALTERED SENSORIUM SECONDARY TO HYPONATREMIA HYPOKALEMIA HYPOCHLOREMIA HYPOCALCEMIA WITH TETANY RESOLVED.METABOLIC ALKALOSIS WITH CHRONIC COUGH (SINCE 4 YEARS)WITH NORMAL CHEST X RAY WITH POSTURAL DROP ?ADDISONS DISEASE ?ADRENAL KOCHS ?ENDOBRONCHIAL KOCHS WITH PRERENAL AKI -RESOLVED WITH
TREATMENT:
INJ 3%NACL 10ml/hr IV
IVF 500 ml NS +2 AMP KCL OVER 5 hrs
INJ ZOFER 4mg IV/BD
INJ PAN 40 mg IV/OD
IVF 0.9 %NACL @ 75 ml/hr
INJ CIPROFLOXACIN 400 mg IV/BD
SYP LACTULOSE 15ml PO/HS
T.OLANZAPINE 2.5 mg PO/BD
T.OROFER XT PO/OD
INJ CALCIUM GLUCONATE 6 AMPOULES IN 500 ml NS@40 ml/hr
T VIT D3 60k ONCE WEEKLY
T PHOSPHORUS 40 mmol/ day
I/O CHARTING
MONITOR VITALS HRLY
BRIEF COURSE IN HOSPITAL:
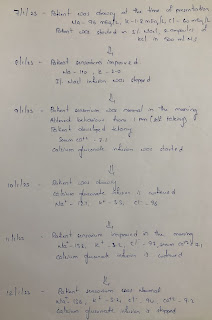
On 7/1/23 :PATIENT WAS LETHARGIC AT THE TIME OF PRESENTATION. Na- 96 , K -1.8 , cl - 60mEq/lit PATIENT WAS STARTED ON 3%NACL @ 10ml/hr AND 2 AMPOULES OF KCL IN 500 ML NS AROUND 8.30 PM.OBG CONSULTATION WAS TAKEN I/V/O CYSTOCOELE.PACKING WAS DONE.
On 8/1/23:PATIENT WAS ORIENTED TO TIME ,PLACE,PERSON .Na - 110 , K-1.8 , Cl - 683% NACL WAS STOPPED AT 9PM2 AMPOULES OF KCL IN 500 ML NS IS GIVEN ABG : PH -7.57 PCO2 - 39.3 PO2 -78.8 HCO3-36.9
On 9/1/23:PATIENT WAS ORIENTED TO TIME,PLACE,PERSON IN THE MORNING . Na -123 K- 2.2 Cl-802 AMPOULES OF KCL IN 500 ML NS IS GIVENPATIENT DEVELOPED ALTERED BEHAVIOUR FROM 1Pm (SELF TALKING).PSYCHIATRY OPINION WAS TAKEN AND PATIENT WAS GIVEN T. OLANZEPINE 2.5 mgNa -130 K-2.8. Cl-90ABG : PH -7.55 PCO2 - 38.8 PO2 -79.6. HCO3-34.3
On 10/1/23:PATIENT WAS DROWSY FROM MORNING Na - 133. K- 3.3. Cl- 96PATIENT WAS GIVEN INJ HALOPERIDOL 1/2 AMPOULE AS PER PSYCHIATRY ADVICE.CT BRAIN WAS DONE TO RULE OUT HAEMORRHAGE >--------------&&-&& INFARCT WHICH TURNED OUT TO BE NORMAL .PATIENT DEVELOPED-------- TETANY SERUM Ca - 7.1CALCIUM GLUCONATE INFUSION WAS STARTED 6 AMPOULES IN 500ml NSABG : PH -7.40 PCO2 - 49. PO2 -148. HCO3-30.4
On 11/1/23:PATIENT WAS ORIENTED TO TIME ,PLACE,PERSON IN THE MORNING Na -138 K- 3.2. Cl- 97 Ca- 7.2CALCIUM GLUCONATE INFUSION IS CONTINUED .ABG : PH -7.47 PCO2 - 41.5 PO2 -88.6 HCO3-30.4
On 12/1/23:PATIENT WAS ORIENTED TO TIME ,PLACE,PERSON Na - 136 K-3.2. Cl- 94 Ca- 9.2 CALCIUM GLUCONATE INFUSION IS STOPPED ABG : PH -7.47 PCO2 - 38.9 PO2 -79.5 HCO3- 28.8PATIENT WAS ADVISED CT ABDOMEN TO RULE OUT ABDOMINAL TB BUT PATIENT ATTENDERS ARE NOT WILLING.
On 13/1/23:PATIENT IS CONSCIOUS, ORIENTED TO TIME,PLACE, PERSON Na - 139 , K- 3.4 Cl- 96 , Ca-8.5PATIENT IMPROVED SYMPTOMATICALLY AND IS DISCHARGED IN A STABLE CONDITION.
PULMONOLOGY CONSULTATION WAS TAKEN I/V/O ENDOBRONCHIAL TB , ADVISED SPU










































Comments
Post a Comment